
Perspective
Amitabh Chandra, Ph.D., Dhruv Khullar, M.D., M.P.P., and Gail R. Wilensky, Ph.D.
A central health care–related policy question for the United States is whether the federal government’s role in financing graduate medical education (GME) increases the number of physicians trained and influences their specialty choices by subsidizing the cost of training. Total federal GME funding amounts to nearly $16 billion annually. Medicare is the largest federal government contributor to GME, providing $9.5 billion — almost $3 billion for direct medical education (DME), to pay the salaries of residents and supervising physicians, and about $6.5 billion for indirect medical education (IME), to subsidize the higher costs that hospitals incur when they run training programs. Federal Medicaid spending adds another $2 billion for GME, and an additional $4 billion comes from the Veterans Health Administration and the Health Resources and Services Administration. States support GME through nearly $4 billion in Medicaid spending.1
The conventional wisdom is that increasing GME funding is key to addressing any physician shortages, will lead to the production of more residents, and reduces the financial burden imposed by becoming a physician. This wisdom results in advocacy for increasing DME funding. But we would argue that DME financing does little to offset the cost of training physicians — that residents essentially pay the full cost of their training, while the DME program simply transfers money to recipient hospitals. IME is more controversial, in terms of both the accuracy of the costs that are reimbursed and the underlying concept — paying institutions more because they spend more, rather than because they provide higher value. Such cost-based reimbursement runs counter to the direction in which health care reimbursement is heading. Moreover, even cost-based reimbursement requires accurate knowledge of costs, ideally marginal costs, but few providers know their cost structure.
In his theory of human capital, Nobel Laureate Gary Becker explains why economists believe that residents, not the hospital where they obtain their training, bear the full cost of their education: they accept lower wages during training that offset training’s significant costs.2 For example, if the total cost of training a resident is $80,000 annually but his or her services generate $130,000 in hospital revenue, then the resident would appropriately be paid a salary of $50,000 — the difference between the two.
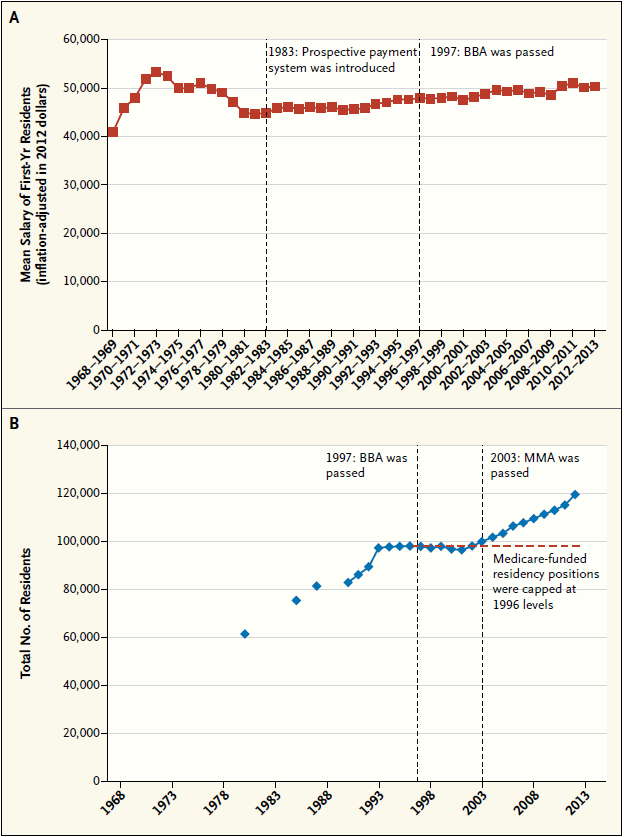
BBA denotes Balanced Budget Act, and MMA Medicare Modernization Act.
The training provided to both medical students and residents is general training — that is, it can be used anywhere — in contrast to specific training, which can be used only at the place where the training occurs. (There may be a small amount of specific training involved — for instance, learning a software package used only at a particular hospital — but that is the exception.) Because general training is so portable, it would make no sense, in purely economic terms, for employers to subsidize its cost; they would not be able to recoup their investment, because once trained, physicians can and do practice wherever they wish. The point is not that general training should not be supplied but that it should not be subsidized; similarly, another job involving a substantial general training component, such as a new MBA’s on-the-job training in reading balance sheets, will have a lower salary than business jobs for which fully trained personnel are hired.
Why are residents paid wages whereas medical students pay tuition? Both receive some amount of training and education and provide some amount of services, but the relative valuation of and time devoted to services received and services provided differs dramatically between residents and medical students.
Medical students provide relatively minor amounts of service, acting mostly as apprentices or observers. They are primarily receiving a costly education in basic and clinical sciences, and they generate minimal revenue; thus, they pay tuition for the education they receive.
Residents receive some direct educational benefits, and their practice during training can incur costs for the hospital; for example, they tend to order more tests and services than fully trained physicians do. But unlike medical students, residents provide substantial amounts of service to patients, thereby generating substantial revenues for their hospitals, particularly after the first year of residency. That residents tend to be paid similar salaries regardless of their specialty or year of training, even though their net contributions vary substantially along both these dimensions, reflects a decision by the institutions to effectively transfer revenues from later years to early years and from more lucrative specialties to less lucrative ones.
This theory is well known to most economists, and there is empirical evidence that strongly supports it. If GME funds were subsidizing resident salaries, those salaries and the numbers of residency positions should have changed when GME funding was adjusted. As the graphs show, however, despite large changes in GME funding, residents’ salaries have remained constant over time; indeed, not only did the number of residents not decrease when GME monies were reduced but it actually continued to increase after several years of adjustment.
In 1983, Medicare introduced the prospective payment system for hospitals and made the distinction between DME and IME. The 1997 Balanced Budget Act (BBA) reduced DME payments by $1 billion (in 2012 dollars) over 5 years and reduced IME payments by $8 billion over the same period.3 These substantial reductions in program funding were not met with any changes in residents’ salaries — a finding that is inconsistent with the claims of teaching hospitals but consistent with those of economists.
The BBA also capped the number of residency positions that would be supported by Medicare at 1996 levels, in order to curb the financial incentive for hospitals to add more residency positions. As the graph in Panel B shows, there was a hiatus in the growth in positions immediately after the BBA was passed, but growth rates returned to pre-BBA levels within 5 years.
We know that hospitals would counter that GME cuts hampered their financial performance and that this poorer performance adversely affected their ability to treat patients. But that claim is inconsistent with the findings of studies that have examined the effects of the BBA payment cuts on patient outcomes: there were no negative effects on mortality rates or process measures of care.4,5
All this evidence is consistent with the view that residents bear the cost of their own training, which would mean that GME funds are treated as general monies going to their institutions; in fact, these funds are often used in ways that are difficult to trace, assess, and justify.
If the policy goal of federal funding for GME training is to alleviate physicians’ indebtedness or to encourage more medical school graduates to go into primary care practice, other strategies may be more effective — such as offering selective loan forgiveness or vouchers to offset tuition for trainees who opt for careers in primary care. Such strategies directly benefit the recipient physician instead of the training institution. Alternatively, if the current training system is not preparing residents adequately to practice using team-based strategies or to focus sufficiently on improving health care outcomes, GME monies could be targeted for activities directed toward those goals, with appropriate metrics verifying the outcomes of the training.
A different justification often given for federal residency funding is that it provides hospitals that treat indigent populations with a needed financial infusion. But with the Affordable Care Act providing coverage for many poor and low-income Americans who were previously uninsured, that justification is substantially weaker than it was in the past.
Ultimately, it is important to recognize that achieving the goals that have been deemed desirable for 21st-century health care will require much more than expanding the GME program under the pretext of solving the physician shortage; we must instead ensure that limited public monies are spent in ways that achieve clearly articulated goals.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
From the Harvard Kennedy School of Government, Cambridge, MA (A.C.); Yale University School of Medicine, New Haven, CT (D.K.); and Project HOPE, Bethesda, MD (G.R.W.).
This article was published on May 14, 2014, at NEJM.org.
- Health policy brief: graduate medical education. Health Affairs. August 16, 2012 (http://www.healthaffairs.org/healthpolicybriefs/brief .php?briefid=73).
- Becker GS. Human capital: a theoretical and empirical analysis, with special reference to education. New York: National Bureau of Economic Research, Columbia University Press, 1964.
- Iglehart JK. Support for academic medical centers — revisiting the 1997 Balanced Budget Act. N Engl J Med 1999;341:299-304.
- Volpp KG, Konetzka RT, Zhu J, Parsons L, Peterson E. Effect of cuts in Medicare reimbursement on process and outcome of care for acute myocardial infarction patients. Circulation 2005;112:2268-75.
- Seshamani M, Schwartz JS, Volpp KG. The effect of cuts in Medicare reimbursement on hospital mortality. Health Serv Res 2006;41:683-700.
DOI: 10.1056/NEJMp1402468
Copyright © 2014 Massachusetts Medical Society.