
Perspective
This past July, after intense lobbying from physician groups, Congress once again stepped in to prevent physicians who provide care to Medicare patients from seeing a 4.5% reduction in their fees.1 Congress appropriately feared the potential problems with access to care that could result from such a fee reduction. But although putting more money into the same broken physician-reimbursement system may buy lawmakers a little more time to address the need for a new one — helpful only if they use it to set the direction for a new system — it also makes the eventual solution even more expensive, since Congress has been providing funding only for the cost of the current year’s fix, not for its ongoing costs. When the latest adjustment craters in January 2010, physicians’ payments are supposed to revert to the lowest level they would have reached had it not been for the temporary patches; this would amount to a 20% reduction in fees. Although it is hard to imagine such a draconian cut actually occurring, it is even harder to envision what Congress is prepared to do in response to this latest threat.
Medicare originally based its reimbursement to physicians, like all its reimbursements, on the amounts that had historically been charged for particular health care services. In 1984, when the program moved away from a charge based per-diem rate for hospitals, it introduced the use of the Medicare Economic Index — a measure of the annual change that physicians face in the costs of practice — for updating physicians’ reimbursement. This change marked
the start of an increasing divergence between Medicare’s reimbursement of physicians and its reimbursement of other providers.
The trend in most Medicare reimbursement has been toward bundled payments. The adoption, in 1983, of a prospective payment system for inpatient hospital care — based on predetermined reimbursement rates for hospitalizations according to the patient’s condition (as classified in a diagnosis-related group, or DRG) — was the beginning of that process, and the bundled approach has since been extended to capital payments for inpatient care, as well as to outpatient hospital care, renal care, home care, and nursing home care. The ultimate in bundled payments is a single capitated payment that covers all Medicare services, such as that used for Medicare Advantage Plans.
There is some concern that provider organizations may seek to boost their incomes by inappropriately increasing volume, providing services to patients who don’t really need them, but this strategy is generally regarded as less likely to succeed with services for which provider organizations receive bundled payments than with those eligible for discrete payments. Moreover, some rules have been introduced to limit the likelihood that providers will try such tactics — for instance, a prohibition on reimbursement for a hospital readmission for the same diagnosis within 30 days after the original admission, although a variety of exceptions are permitted for medically appropriate readmissions.
The history of physician payments under Medicare has taken a rather different path. Though there was a time in the 1980s when the program considered using DRGs to calculate physician payments as well as hospital payments, so far there has been no serious movement in this direction. Bundled payments are used to reimburse physicians in some instances: surgeons receive a fixed payment that covers preoperative care, the procedure itself, and some postoperative care. In general, however, physicians are paid for providing discrete services, according to a disaggregated fee schedule that uses more than 7000 billing codes. In 1989, a major change was made in physician payments: the disaggregated fee schedule based on historical charges was replaced with the Resource-Based Relative Value Scale, which is based on relative values for physicians’ work effort, physicians’ practice expenses, and malpractice liability insurance expenses. Although the scale was intended to correct for a historical undervaluing of primary care and overvaluing of procedures (which it does not appear to have done very successfully) and for larger differences between urban and rural reimbursements than could be justified by differences in the costs of practice, it retained the use of a largely disaggregated fee schedule.
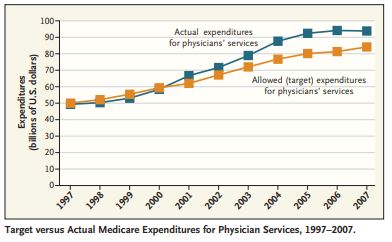
Because the risk of inappropriate volume increases is much greater with a disaggregated billing system, as the experiences of the 1980s showed, updates to the fee schedule have followed a top-down strategy. Since the early 1990s, overall Medicare spending has been tied to a preset target — initially to the volume performance standard (an amount that was set into law each year) and now, through the sustainable growth rate (SGR), to the rate of growth in the economy. Fees are adjusted whenever overall spending is greater (or less) than the target level (see graph).
Most recent discussion of reforming physician payment has focused on the SGR, which has caused the pressure to lower physicians’ fees. Because the use of an SGR mechanism only for physicians forces just one part of Medicare to maintain a rigid relationship to the economy, one option proposed by the Medicare Payment Advisory Commission (MedPAC) is to expand the use of such expenditure targets throughout Medicare.2 Although doing so might reduce the pressure on physicians, it would not address the question of the appropriateness of any given distribution of Medicare spending among the various components of the program. In addition, expenditure targets in and of themselves do nothing to improve quality, ensure clinical appropriateness, or accomplish other Medicare goals.
However, the most fundamental problem with the SGR is that its objective is inconsistent with the incentives it produces. The objective is to control total physician spending. The problem is that the SGR neither affects nor is driven by the spending of any individual physician. If anything, individual physicians are provided with an even greater incentive to increase spending, because nothing they do as individuals can affect overall spending, but their fees will be affected by what other physicians do collectively, irrespective of their own behavior.
A variety of short-term patches, most of them focused on how the SGR is calculated, have been suggested to correct this problem. These include the use of multiple SGRs (reflecting the differences among specialties in the rate of spending growth) and the use of separate SGRs for multispecialty group practices (encouraging the development of more such groups, which have been associated with high clinical quality and appropriate financial incentives).2,3 A different way to reduce physicians’ spending, and thus some of the downward pressure on physicians’ fees, is to have the Centers for Medicare and Medicaid Services (CMS) more aggressively review billing by physicians who are clear outliers in terms of their use of medical procedures and ancillary services, a strategy that appears to be permitted under the Medicare bill that Congress passed in July 2008.
Although all these approaches might provide some short-term relief, I believe the key to reforming physician payment is to develop a more aggregative payment strategy. In the near term, payments need to be developed that cover all the services that a single physician provides to a patient for the treatment of one or more chronic diseases. This approach is consistent with, and could be related to, the work that CMS and others are doing on medical homes. In addition, bundled payments should be developed for high-cost, high-volume DRGs, to include, at a minimum, the reimbursement for all physician services associated with the DRG and perhaps the hospital payment as well. For example, a single payment could be made to cover all physician services and hospital care related to coronary artery bypass grafting, rather than having each physician bill Medicare separately. In the 1990s, a demonstration of such bundling was conducted by the Health Care Financing Administration, the predecessor to the CMS. The results were promising in terms of clinical outcomes and savings, but as often happens with demonstrations, no further movement has occurred.
At the same time that any interim steps are being taken, I think the CMS should move ahead with a two-part request for proposals — one part for the design, one part for the implementation strategy — that would result in a more fulsome redesign of an aggregated physician payment system. It seems clear that although various models for payment reform are in development, none are currently ready for full implementation by Medicare.
There is no quick fix for physician payment reform. Under the most optimistic of scheduling scenarios, the implementation of a redesigned system is unlikely to occur before January 2013. The first quarter of 2009 is none too soon to start.
No potential conflict of interest relevant to this article was reported.
Dr. Wilensky is a senior fellow at Project HOPE, Bethesda, MD, a former administrator of the Health Care Financing Administration (now the CMS), and a former chair of MedPAC.
- Medicare Improvements for Patients and Providers Act of 2008 (MIPPA). Baltimore: Centers for Medicare and Medicaid Services. (Accessed January 23, 2009, at http://www.cms.hhs.gov/apps/media/press/release.asp?counter=3200.)
- Medicare Payment Advisory Commission. Report to the Congress: assessing alternatives to the sustainable growth rate system. March 2007. (Accessed January 23, 2009, at http://www.medpac.gov/documents/Mar07_SGR_mandated_report.pdf.)
- Berenson R. Options to improve quality and efficiency among Medicare physicians: testimony before U.S. House Ways and Means Subcommittee on Health, May 10, 2007. (Accessed January 23, 2009, at http://www.urban.org/publications/901105.html.)
- Rosenthal MB. Beyond pay for performance — emerging models of provider-payment reform. N Engl J Med 2008;359:1197-200.
Copyright © 2009 Massachusetts Medical Society.